Spotlight on Heart Mapping Technology in Electrophysiology
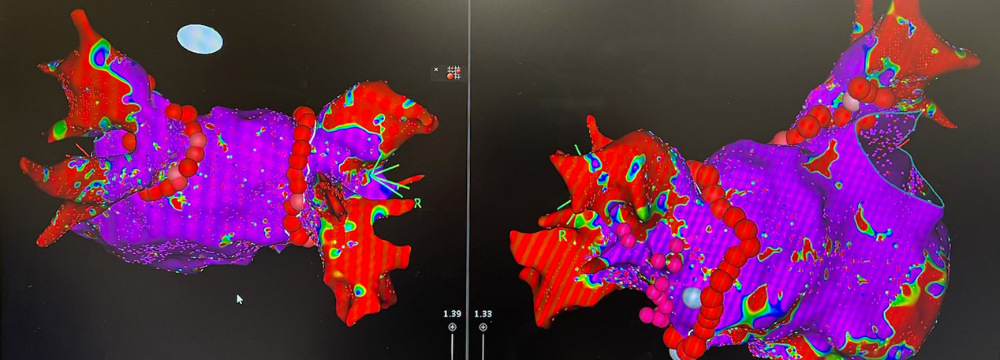
You may remember a prior post on our website discussing the incredible technology we, as electrophysiologists, have at our fingertips. This technology has made treating cardiac arrhythmias, particularly Atrial Fibrillation or Afib, safer and more effective than ever. Another significant benefit of this technology is the time it takes for Dr. Moretta to complete an ablation. What once routinely took 2, 3, 4, or more hours can now be performed in less than an hour and often in as little as 45 minutes. One of the key technological features of any advanced electrophysiology lab is the three-dimensional mapping we use to visualize the structures of the heart and the path and amplitude of the electrical signals that may be causing the arrhythmia. To illustrate this, please have a look at the image below. This is an actual map of the heart of one of our patients enrolled in the REAL-AF study, for which we are a study center. He was the 100th patient we treated for this trial.
You’ll see a few exciting things on this map. First, the detail is incredible. Using advanced technology nestled into the tip of the catheter, we get a real-time picture of what the heart looks like and what it’s doing. This gives us a few key data points that make the procedure more effective and allows us to perform it more quickly.
- First, we can see where the electrical amplitude of the heart varies. A normal heartbeat without an arrhythmia would yield a completely purple image. As you can see, we have red, green, and blue hues consistent with an arrhythmia, particularly Afib.
- This map also allows us to evaluate the results of the ablation strategy in real time. While it can take some time for the arrhythmia to subside after catheter ablation, seeing how the heart reacts to each treatment, as we treat it, is critical to helping us along during the procedure.
- Also, you can see where there are bracelet-like red dots around blood vessels. These represent the ablated areas, and the blood vessels are the pulmonary veins. Pulmonary Vein Isolation (PVI), as it’s called, is a gold standard ablation strategy, so we will follow this pathway for most patients with a similar diagnosis.
As an aside, there are some other genuinely stunning technological advances built into this catheter and mapping technology. These include:
- Stability features to precisely control the catheter
- Measurement of the distances within the heart to the tiniest degree
- Pressure feedback so we know exactly how hard we are pushing on tissue
- Visual representation of the angle of the catheter
We can even reference prior procedure milestones and import them into the map.
As you can see, technology plays a significant role in how an electrophysiologist does their job. It’s one of the reasons why patients often get frustrated at their primary care physician or cardiologist’s office if they don’t get a satisfactory answer about a complex arrhythmia. From the diagnostic process to follow-up after a procedure, employing an experienced electrophysiologist is the best way to ensure a proper diagnosis and a treatment plan that addresses your needs. We encourage you to call our office to learn more and schedule a visit with Dr. Moretta.